Occupational Therapy
It's OT Month! Celebrating the possibilities
Nothing is impossible, the word itself says ‘I’m possible’!” – Audrey Hepburn
Don’t you think that’s a great quote for OT? I’m not saying someone with a cervical spinal cord injury should be walking, just that there are always possibilities, some of which we don’t even even know we don’t know. Occupational therapists are often blessed with knowledge that allows them to shed light on new possibilities for those facing the seemingly impossible. One of the most beautiful parts of our job. Watching faces light up with new understanding, new awareness, a sense of possibility, a sense of hope. A sense of future.
It’s April, and it’s OT Month. A month were we celebrate the possibilities and our role as OTs in their illumination.
Lately I haven’t been blogging quite as much, I’ve been posting a lot on Twitter over at https://twitter.com/msawesomenessOT and on Facebook at https://www.facebook.com/missawesomenessdotcom
You can also see them on my blog sidebar.
Speaking of impossibles, I’ve been doing a lot of rock artwork lately, and I’ve gone from stacking flat rocks (the cairns) to working on vertical rock balancing. I balanced these rocks – they’re actually only a few inches tall – on bigger rocks over at Torrey Pines State Beach in La Jolla, CA. I’m proud of it! Very challenging yet calming, meditative. Helps my swirling mind feel at peace. I never, ever would have thought it was something I could do!
The Possibilities and Potential with an OT degree :)
Many people get degrees (history, art, religion, technology) then have NO idea what to do after graduation…it doesn’t necessarily feed into any one profession. They have so many possibilities, but first they have to figure out what to do next.
In occupational therapy (OT) or occupational therapy assistant (OTA) school, you know you will become an occupational therapy practitioner afterwards. It’s a “confined diversity” in that you aren’t going to sit around wondering, gee, what will I become when I graduate? That’s a great thing about clinical degrees.
And yet then your possibilities become remarkably diverse, once you’re an occupational therapy practitioner. You can work with newborns or those at the end of their life or anywhere in between. You can work with people who are completely healthy. You can work with people with physical challenges or mental health challenges, either congenital or acquired. There’s just no limit to what you can do. That’s what I love about OT. It let me go into a specific profession without any wondering, yet then opened up the skies so that I could do anything. 🙂
Just thinking out loud!
Can observing a client in one context allow us to predict ability in another?
I created this scenario to explain how, for example, assessing “Mary’s” ability to get ready in the morning (her “occupational performance”) can tell me a lot about her likely performance in making a simple meal.
(A modification of this would be great to use with OT/OTA students in the classroom or on fieldwork. Sharing how Mary does in her morning routine, then asking them to predict what she would be like in the kitchen.)
Mary is a 75-year-old woman who wants to be able to independently make a simple meal, while using hip precautions, her walker, and energy conservation techniques. She is currently in inpatient rehab. If we [OTs] work with her during her morning routine , even if we haven’t seen her in the kitchen yet, we will learn valuable information to predict how she would do in the kitchen. We may see she is forgetting to use- or doesn’t understand- her hip precautions. We may see that she is inefficient in her method, walking back and forth across the bathroom to get one item at a time. That she sequences tasks incorrectly, putting on makeup then realizing she hasn’t washed her face. That she is unsafe, with seemingly no awareness of fall hazards or an ability to remember to turn off her curling iron. All of these components will demonstrate to the OT that she may not be ready to safely make a meal by herself that involves anything that needs to be turned off, and that she may need items grouped together for efficiency reasons, such as keeping the peanut butter, jelly, bread, and a butter knife all in one area. She may also benefit from a written or visual list of instructions. We haven’t even seen her in the kitchen yet, but by watching her in the bathroom, we already have information that will guide our intervention and possibly fill in some of the blanks on an assessment tool. There are many safety similarities between getting ready in the morning and making a meal, as it pertains to slippery surfaces, heated objects, sequencing, underlying skill deficits both physically and cognitively, etc.
*I’m using more laymen terms here for easier understanding, but in medical documentation I would use more professional terminology
*Born out of a discussion in one of my post-professional OTD classes, involving assessment of various occupational performance areas.
(Prediction of occupational performance in varying activities of daily life (ADLs)
Mental Health Energy Conservation
How do adults (18-55) with mild depression describe their energy expenditure as it relates to participation in activities of daily life?
My review of the literature came up with no results that specifically focused on energy expenditure in relation to mental health and activities of daily life. The majority of articles focusing on energy conservation had to do with multiple sclerosis (Blikman, et. al, 2013), cancer (Mitchell, et. al, 2014), or other physical difficulties. Other articles focused on older adults and limitations in activities of daily life in the aging process, which occasionally addressed depression (Arbesman & Mosley, 2012). Others address activity limitations and depression with chronic conditions, but do not specifically focus on mental health. While I may have missed some articles in my non-exhaustive literature search, it’s clear that this is a very specific area that has had minimal attention.
Occupational therapists and many other health professionals have knowledge and experience in dealing with energy conservation, but it’s typically based on physical needs, not mental. Mental health occupational therapists clearly recognize that people with depression have limitations in ADLs, and that even an activity as benign and simple as pouring a bowl of cereal can seem exhausting. While they certainly address these issues, I don’t know if the therapists or clients are considering this or calling this a form of energy conservation. It would be interesting to see if adults with depression describe their energy expenditure for such tasks as physical or mental, or even perceive the limitation as an energy expenditure issue in the first place.
I think the occupational therapy field would benefit from a more evidence-based approach to managing energy conservation in younger adults with mental health challenges (I chose depression but I’d also be equally interested in anxiety). If there were an assessment that was linked to the COPM, it would allow the therapist and client to get the unique viewpoint of what activities take up the most energy expenditure for that particular client (emphasis on uniqueness), and give them goals for intervention. A support group and/or energy conservation program could also be appropriate for this population.
Occupational therapy is rarely seen in most major healthcare mental health settings these days, but mental energy conservation programs for ADLs could be a new way to promote OT in mental health, and a way to help more people handle their day to day ADL participation with more awareness, compassion, and knowledge, which may in turn reduce their limitations and allow increased participation.
References
Arbesman, M., & Mosley, L. J. (2012). Systematic review of occupation- and activity-based health management and maintenance interventions for community-dwelling older adults. American Journal of Occupational Therapy, 66, 277–283. http://dx:doi.org/10.
Blikman, L. J., Huisstede, B. M., Kooijmans, H., Stam, H. J., Bussmann, J. B., & van Meeteren, J. (2013). Effectiveness of Energy Conservation Treatment in Reducing Fatigue in Multiple Sclerosis: A Systematic Review and Meta-Analysis. Archives Of Physical Medicine & Rehabilitation, 94(7), 1360-1376. doi:10.1016/j.apmr.2013.01.
Mitchell, S. A., Hoffman, A. J., Clark, J. C., DeGennaro, R. M., Poirier, P., Robinson, C. B., & Weisbrod, B. L. (2014). Putting Evidence Into Practice: An Update of Evidence-Based Interventions for Cancer-Related Fatigue During and Following Treatment. Clinical Journal Of Oncology Nursing, 1838-58. doi:10.1188/14.CJON.S3.38-58
The Amazing Breadth of Occupational Therapy!
As occupational therapists, we are so lucky to have training that allows us to to help any person of any age and with any issue, by addressing the factors that are hindering their ability to participate as fully as possible in their own life! OTs learn to analyze the spectrum of possibility and then help the supposed impossibles become possible.
Here are some of the areas we work in:
OT & Schools (children in any grade who need services for their particular issue…sensory, handwriting, fine motor, visual motor, regulation, tolerance, executive functioning…)
OT & Mental Health (of any age after mental health challenges become apparent, helping with independent living, tolerance, regulation…)
OT & Pediatrics (children of any age and any diagnosis)
OT & Acute Care (immediate care after acute issue)
OT & Inpatient rehabilitation (regaining function in a facility after hospital stay for any issue…)
OT & Outpatient (helping huge variety of issues)
OT & Vocational Rehab (for first time, back to work, or finding new work…)
OT & Driving (getting on or back on the road, safety…)
OT & Hands (trigger finger, lateral epicondylitis, accidents, burns…)
OT & Feeding (children and adults with special needs)
OT & Neurology (strokes and multiple sclerosis…..)
OT & Orthopedics (hip and knee and much more…)
OT & Chronic Disease (diabetes, lung diseases, pain syndromes…)
OT & Military (amputations, PTSD and much more…)
OT & Trauma (burns, pain management, catastrophic injuries…)
OT & Health and Wellness (joint protection, ergonomics, energy conservation, self-care, empowerment, fall prevention…)
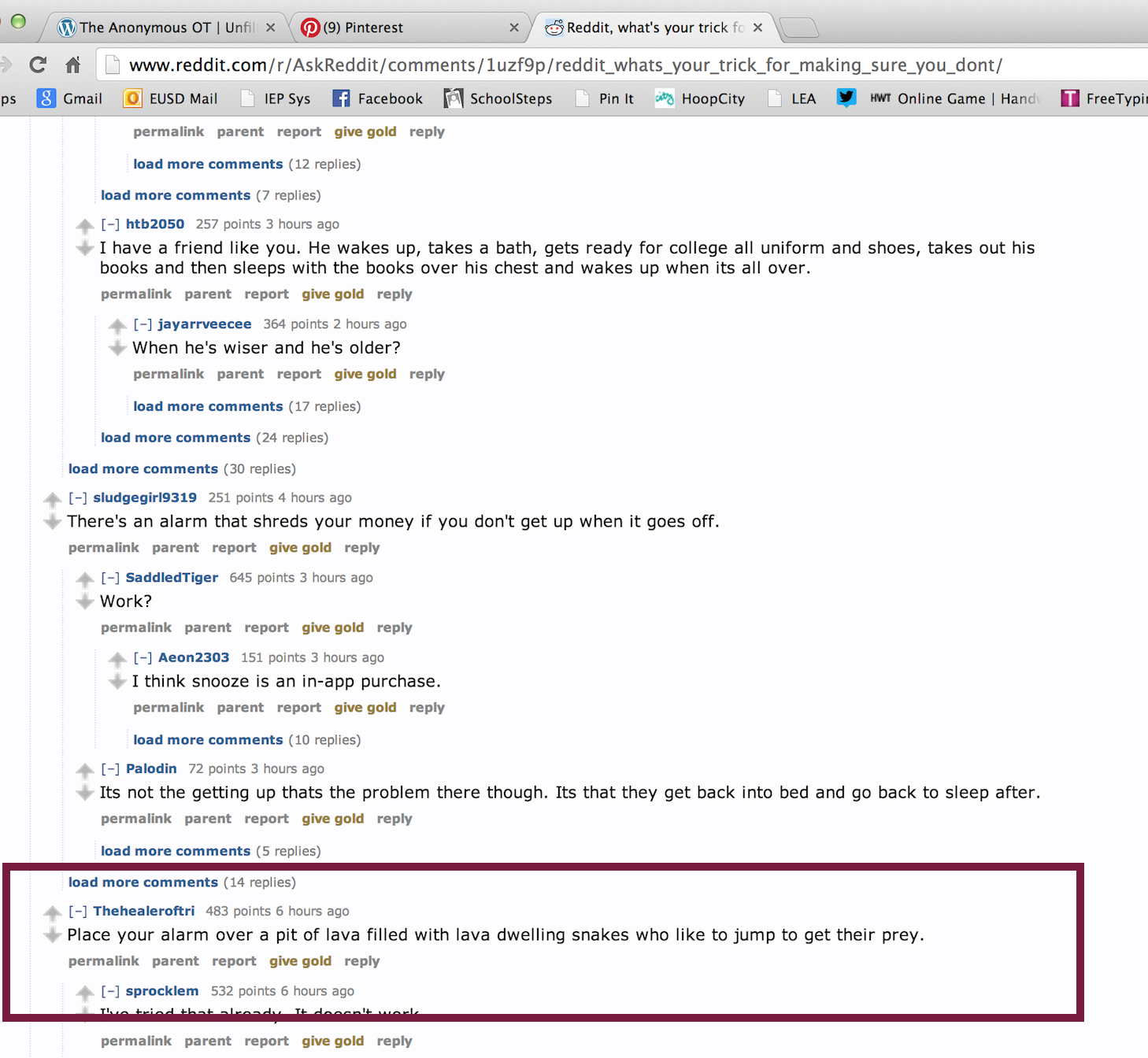
Let's hope this man isn't an OT
I cracked up at the screen shot below. It was a Reddit.com thread about methods to get up in the morning. Redditors are notoriously snarky. I loved the bolded box below. The man’s suggestion was to "place your alarm over a pit of lava filled with lava dwelling snakes who like to jump to get their prey." Yes, that would certainly wake a person up. OTs can work with sleep hygiene although most of us don’t take it quite that far. 🙂
PS: I recommend going to Reddit and checking the "Ask Reddit" section because they have some pretty incredible topics, some of which may be helpful to occupational therapists.
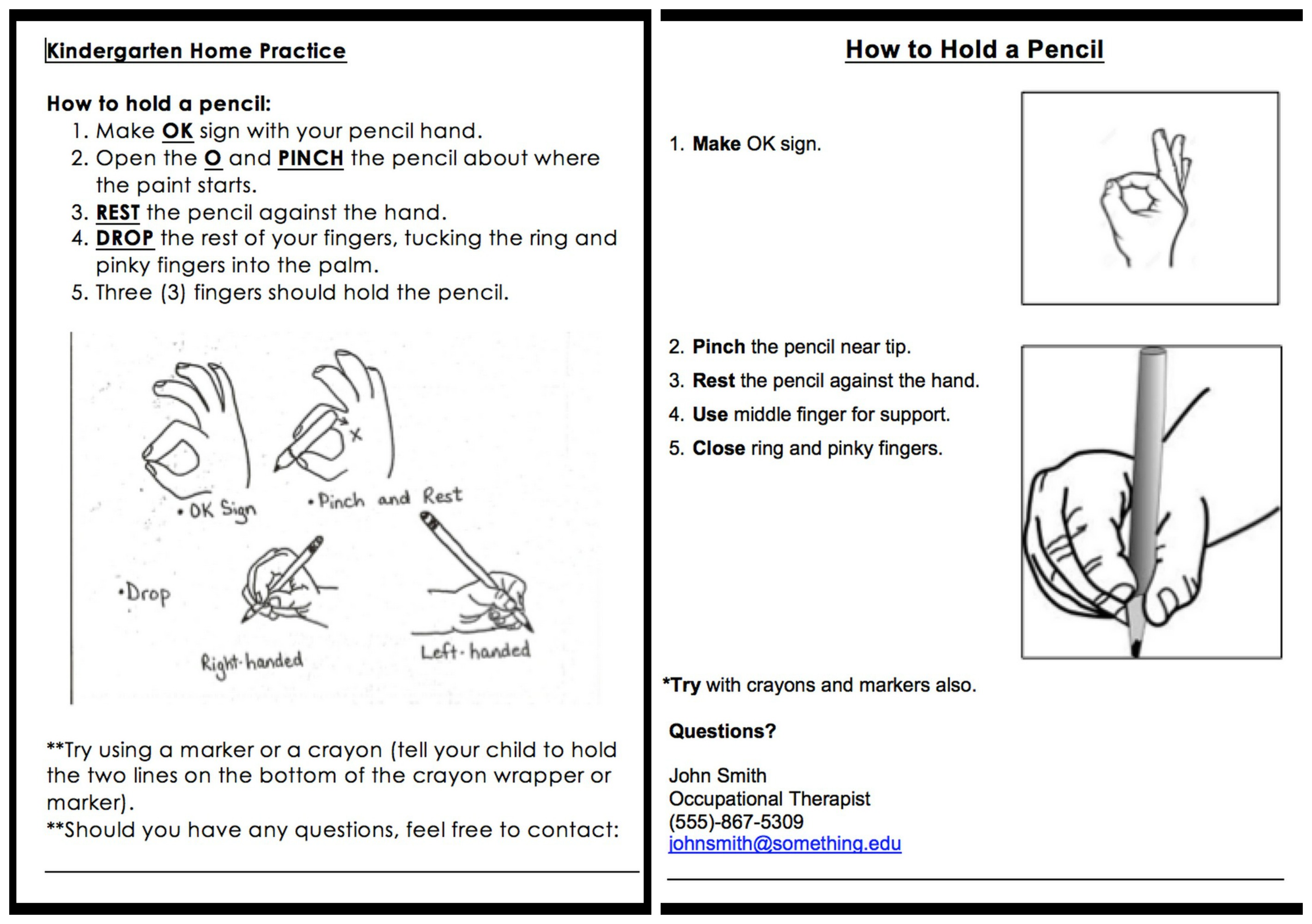
Health literacy and educational hand-outs
Educational handouts to clients should rarely be above an 8th grade level, and often more like 4th grade. Here is a "before" and "after" of a handout that some of my classmates and I modified in our Education in OT course!
Four of us modified it in a small group assignment. We all just got back from our once-a-semester 3-4 day onsite visit at the Rocky Mountain University of Health Professions campus, based in Provo, Utah.
*I’m getting my post-professional clinical doctorate in occupational therapy through their program, which is mostly online. I find the curriculum rigorous yet reasonable, and the professors awesomely hysterical yet wonderfully knowledgeable and helpful. I’m really enjoying it as a form of vocational rehabilitation, opening new and non-traditional doors for me, so that I can be a successful occupational therapist even if I can’t handle daily regular direct service sessions!
Remembering our upbringings affect our expectations of clients
Just thinking out loud/reflecting here. 🙂 I really enjoyed reading the following Facebook post by F.C. on the group page, “Pediatric Occupational Therapists”. (I recommend joining this group, a lot of high-quality information and resources.) I enjoy outside-the-box thinking and creativity, and at times I felt guilty trying to reconcile my work with some of the more rigid academic necessities. I did have a typical schooling so I understand “normal” expectations, but I think more like F.C.!
“I went to a very small alternative school from 1st grade through high school that really emphasized individuality and creativity. It was a wonderful place to be and we learned a lot of great life skills, but there was no OT and no one was too concerned with typical development. Fast forward 20 years and I am at my first fieldwork placement at a peds clinic, working with a little boy who was coloring. He was having a great time and using a bunch of different colors and free form drawing before he filled in the shapes… My supervisor (who is lovely) walked in and called him out on not coloring properly – oops! I had no idea up to that point (as a 30 year old) that coloring is usually supposed to be one color, fill the whole area systematically, etc. I thought this kid was doing great! It was an interesting reminder that my upbringing is always going to affect the way I see things and the way I treat. I’m still not sure of everything kids are “supposed” to be doing at certain ages, except out of text books, which don’t give us much.”
Controversy: Patient versus Client versus Consumer?
Patient, Client, or Consumer? In occupational therapy and other healthcare fields, there is a semantic controversy over what us therapists/the public should be calling those who utilize occupational therapy services. Depending on the label used, we get a different feel for the relationship between therapist/person.
My friend, a psychologist, told me she likes to use the word “patient” because it came from Latin and means “one who suffers,” and she feels the people who see her are there because they are suffering. Some therapists prefer “client” as they feel “patient” has more of a superior-inferior feel, as well as a “medical model” feel, and many OTs feel we need to be more encompassing. Other therapists prefer “consumer” because it seems to have a more neutral connotation. I’m sure there are plenty of other reasons for the different labels. Some therapists feel very passionately about the “appropriate” label, others don’t really care, others use them interchangeably. I think there may be an even better label out there. Hmm. So I just asked my pediatric therapist friend what she calls the people she sees, and she said with a shrug, “child.” I loved that answer! Maybe that’s the best one of all. 🙂
What do you think? Patient, client, or consumer?
Remembering our patients in a larger context
As an occupational therapist who has worked in physical dysfunction, this picture of a senior woman in a hospital, cuddling a cat, really struck me. It’s a reminder that our patients, often seen in a hospital setting with no external context, are real people, with real stories, and real lives. Never forget.

*Picture came off some random site a long time ago – no idea where.