Easy Ways to Teach Your Child Problem-Solving Skills
Does your child get upset easily over small and easily fixable things, like a ball rolling under a table? It may be because he doesn’t realize he has any power to fix the problem. Luckily, you can teach him to feel more empowered. I introduce to you the PSST Method!
Download the PDF of this here: The PSST! Method: Teach Your Child How to Problem Solve
Or just read on.
The PSST! Method: Teach Your Child How to Problem Solve
Children who feel confident in their problem-solving abilities can better tolerate and handle unexpected events. All children of any age can benefit from learning problem-solving skills. Adjust your language or extent of experimentation based on your child’s age/ability/tolerance level. The steps stay the same. (Ideally, use them all in order. But using any is great.)
SAMPLE PROBLEM: Young John’s ball just rolled under the couch. John scrunches up his face, ready to cry. Daddy jumps up to go grab a broom handle and solve the problem.
WAIT! John needs to learn the steps BETWEEN the problem and a successful solution.
- Pause. Just briefly. See if the child will attempt to problem-solve. If not, proceed to step two. Eventually, your child may make the attempt.
- Frame the Problem. “Wow, the ball rolled under the couch, and we can’t reach it.” You can also provide “emotion” and “help” words. “Your face is turning red and you look really frustrated. You can say, “Please help me solve this problem.”
- Play “Dumb.” Whether you instantly have a solution or not, you can pretend you’re not quite sure what to do. Crinkle up your forehead and look thoughtful. “Hmmm….”
- Think Out Loud. Most adults problem-solve in their heads. If you can role-model the problem-solving process, you’re giving him valuable insight, and showing that it’s not magic. “The ball’s is under the couch. We have to get it out somehow…maybe we can try…” With an older child, you can ask them if they have any ideas.
- See What Happens. You may know that your hand won’t fit or his arm can’t reach, but he doesn’t. When it’s feasible to experiment (not a safety hazard or massive inconvenience), try it out. He learns a lot more that way. “Let’s see if your arm is long enough. Can you lie down and reach for it?”
- Repeat Steps # 4 (Think Out Loud) and #5 (See What Happens), until problem solved. “That didn’t work because the ball’s too far away, will my hand work? …No, too big. Hmm, maybe something small but long to help us get the ball.. see if this will work…no….hmm…let’s see if we can find something…oh, let’s try a broom handle!”
- Frame the solution. “The ball rolled under the couch and we were really frustrated and we didn’t know what to do. But we tried lots of ways to solve the problem and now we have our ball back. We are great problem-solvers!”
Repeat this process regularly. As he becomes more proficient, you can take more of a back seat to the problem-solving process.
Bonus: Consider sprinkling “What If’s?” into your conversations/play time. “We solved that problem! What if the ball landed in a tree? Or this hole? Or under the bed?” Talking is great, acting it out is even better. Play a game called “Problem-Solving Superheroes” where you deliberately practice these kinds of things.
Good luck – let me know how it goes!
PS: This method may seem obvious to you – but many caregivers would benefit from the reminder.
Interested in practical adaptive equipment design?
See flyer here:
Homemade Customized Adaptive Equipment
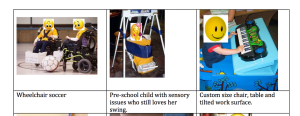
My lovely friend Beth has been working on practical adaptive equipment – creating it at a fraction of the cost of commercial design. I copied the following text from the flyer: “I want to customize or build adaptive items for children with special needs. My dream is to have a workshop where families, teachers and designers can meet. Footrests, booster seats and supportive seats can be purchased from special needs catalogs but they are generally hundreds of dollars. I make most items out of extra strong cardboard, plastic, fabric and foam. They are inexpensive, light-weight and last a long time. I took cardboard construction classes at the Adaptive Design Workshop in New York City. The founder, Alex Truesdell, won a McArthur Award for her work. Many students who take the class are interested in starting their own workshops. It really helps to have experience building things.
What products do your kids need most? What features do you need that you can’t find? What do you want but can’t afford? I would love to hear your ideas. I’m not in business yet. I just learned that product liability insurance costs a minimum of $3500 per year. (On top of general liability insurance.) I may have to find or create a position at an existing company or organization that already serves the special needs population. Apparently, the price of insurance is stopping many of my fellow students. Connections are welcome!”
Her contact information is provided in the flyer. If you have any interest in adaptive design, or want some ideas or to know more about her work, you should definitely connect with her.
Poem on retrogenesis
Retrogenesis is the process of people with Alzheimer’s/dementia reverting back to childhood stages..as dementia progresses and more brain cells are ruined, the earlier the stages…I wrote what’s below in 2008. Just stumbled across it again. I’m not a poet, I realize it’s not a masterpiece, but I like some of the concepts…body flowing forward, mind flowing backward. And tabula rasa, at beginning and end. Okay, not exactly, but you get the general idea. 🙂 Maybe it will give you something to think about.
Retrogenesis
When you look at me
What do you see?
An old woman
Or a young lady?
I am both.
My body flows forward
My mind flows backward.
I feel young
Others say I’m old.
That old lady in the mirror strains to see
But that is not me.
I don’t understand why my body fails
When my mind tells me I am so able.
The walker in my hands cannot be mine
I walk with a youthful upright stride.
My mind crackles with static;
time becomes dynamic.
One minute here, one minute there.
I am falling through time
One year two year three year four.
Thirty years forty years fifty years and more.
Now I’m back in childhood, happy and serene.
The years tick back to infancy
as my slate gets wiped clean.
The tabula rasa, beginning and end.
OTs as Detectives: Problem-Solving Dementia-Related Behavioral Triggers
Description: Many people with dementia demonstrate a pattern of behaviors that are perplexing and risky. It turns out there is often a trigger causing the issue. Occupational Therapy (OT) Practitioners are great at investigating the issue, then finding & removing the trigger, therefore extinguishing the behavior.
(I am on a Gerontology Listserv for Occupational Therapists (through the American Occupational Therapy Association), and I’ve gotten to read some really interesting posts lately by OTs about behavior in dementia they have encountered in practice, and how even bizarre behavior typically has a trigger that can be figured out.)
Example 1: There was a woman who kept on climbing on her chest of drawers and was at a high risk for falls, obviously. The OT assessed the situation and found out it mostly happened in the afternoon, and observed the woman. It turned out the woman’s roommate had a crystal in the window and around 2pm the sun would hit it in such a way as to make a kaleidoscope of dazzling colors on the chest of drawers. This was the trigger for her climbing. The crystal was moved and the problem was solved.
Example 2: An older man who fell constantly. The OT did research and discovered he loved biking. She also discovered that he needed a lot of vestibular input and sensory integration-based interventions, or he’d start trying to self-stimulate and would end up falling.
Example 3: A man always groped his caretaker at nighttime during bath time. It seemed like a huge problem, but the OT discovered that historically, the man had always bathed with his wife at night before lovemaking. By moving the bath to the morning, the problem was solved.
Basically, the OT is often an investigator. There were other stories involving men urinating in potted plants and the like. I really liked the discussion because they talked about validation theory, retrogenesis, behavioral triggers, and more. It’s amazing to me.
*I originally wrote this way back in 2008…just stumbled across it again.
Deciding what to teach my OTA students in a mental health course…
As I prepare for the mental health course I’m teaching in the Fall to OTA students (my first), I find myself consistently going back to my OT blog. I wrote over a thousand posts (not all of them high-quality, cough) while in grad school (2007-2009) and during my nine months of full-time internships, which included three months in a geriatric psych ward. I see all sorts of tidbits that remind me of things I want to share with my students! Things I wish I had done differently, or wish I had known, or need to cover…and I shake my head at some of the stuff I said/wrote. Blogging is a powerful tool for charting growth/the learning process! And if anyone wants to message me with things they wish I could cover…would love to hear your feedback.
To see more posts from grad school days, go to my sidebar and scroll down until you see Archived Posts…right click on one of those years and say Open in New Tab….below is a post I wrote in 2009 about me and a geriatric patient having the same underwear, and a bunch of other random things. 🙂
Is it bad if me and my geriatric patients have the same underwear?
Encouraging Self-Advocacy in Young Children
In my (former) work as a school-based occupational therapist, I was saddened daily at the lack of self-advocacy in the majority of the children I was treating. I provide the following as a (fictionalized but typical) scenario where I help teach self-advocacy.
The background information: Sam is 6 years old and in first grade. He spent two months in the NICU due to prematurity and gastrointestinal issues. He has mild motor developmental delays. He is small and adorable, and everyone feels protective of him. His parents, teachers, and peers are always quick to do things for him. He is cognitively intact, although his executive functions have been somewhat blunted through his early learned helplessness, the passivity that accompanies it, and the compensation by people in his environments. He is uncertain of his own abilities. He receives OT once a week through the school system.
Scenario: Sam is sitting at the table. I hand him a piece of paper and tell him to “sign in” (which he does every week). I deliberately turn away and start rummaging through things, clearly busy. After about 30 seconds I turn around and he is still sitting there, and hasn’t signed in.
“Sam, why didn’t you sign in?” I ask.
“I didn’t have a pencil.”
“Oh!” I say in over-exaggerated surprise. I dramatically retrieve a pencil for him “Next time, please tell me right away that you need a pencil!”
We move on.
Next week, I repeat the scenario. I hand him his paper, tell him to sign in, and start to turn away.
This time, he instantly says “I need a pencil!”
I smile and super happily say “Oh! I forgot! Thanks so much for asking! Here you go!”
We continue to work on similar examples each week. Often I am distracted or make lots of mistakes! Luckily, he helps me stay on track by letting me know what he needs.
Sam, like many consumers, was unaware of his power to ask for what he needs. With guidance and education, he is learning how to be a self-advocate.
The ethical issue of productivity in healthcare
I haven’t blogged in a loooong time and as I was going through old files, I found something I had written about “productivity” within healthcare and the ethical issues I have with it, as an occupational therapist.
Essentially, many hospitals/clinics/settings have a set amount of “productivity” (billable units of time, typically in 15 minute increments, and usually only gotten during client treatment time) that each therapist is expected to get each day. Now, of course productivity can be a good thing in that obviously we want occupational therapists treating clients versus sitting around eating bon-bons, but the reality is that most therapists are already rushing around all day, doing their best to see all their clients, do paperwork, schedule things, collaborate, etc. What I’ve found is that unrealistically high productivity standards tend to lead to ethical dilemmas.
Here’s an example I give, which I experienced during fieldwork in 2009:
I am working on a locked geriatric psych ward. I just finished up an occupational therapy treatment session with a very mobile male who frequently gets aggressive (throwing chairs in hallways and such). He has a short fuse and if he gets stressed/frustrated, he escalates. I’m supposed to meet productivity units and my time is very limited for the rest of the day. As I am walking out of his room where he has gotten into bed, he asks me for a drink of water. Patients can’t get it themselves. I hesitate and the following goes through my brain:
Scenario 1: I get him the drink of water as requested. It will require me heading down a long hallway and navigating multiple people who want my attention, tracking down a nurse for a key, going into a room and getting the water if there are even cups in supply, finding the nurse to return the key, and walking back. He may expect that it’s a simple request, but even if everything goes smoothly, it could take 5 minutes, and possibly closer to 15. I will lose at least one precious, precious unit, but at least he got a need meet as soon as possible and on first request, which means he will -more likely – stay calm. (Why it takes so much work to get water is a separate issue not addressed here!)
Scenario 2. Worst case scenario plays out. I don’t want to lose my productivity so I let him know I have to run but I will ask a nurse as I am headed out. It may be true, but I know full well the chances are extraordinarily high, thanks to strained resources, that the nurse will take mental note and get to it when she can, which may take a while, and that in the meantime, every time anyone walks by his room, he will ask whoever that is again, who will say they will tell his nurse, and he will become increasingly frustrated. Here he is asking for the simplest and basic of needs to be met and nobody will help him. He will escalate to violence, throwing chairs in the hallway as he tends to do. (There’s only one hallway/entrance – no way to get out if he’s blocking it) All other residents will be stuck inside their rooms as area staff deal with this. Now there are six people focusing on de-escalation. In the meantime, patients are stressed, nurses run behind on meds, and I may be stuck somewhere, having to wait until the coast is clear. Now all the employees have lost productivity, quality of care is suffering as now all the poor patients have to deal with this. And it’s certainly not fun for the agitated patient, either. And even if I had already left the area so it didn’t affect MY productivity, it was certainly horrible for those left behind.
IF I DO SCENARIO 1: I get him the water, no escalation, everything stays more or less on track, and I have lost a unit with no good reason (in director’s eyes), which I may get scolded for later. The director doesn’t appreciate hearing “Well yes I didn’t get that unit but it’s because if I didn’t get him his water then X would occur then Y then Z so really I saved units.”
IF I DO SCENARIO 2: I don’t get him the water. I potentially get my productivity unit. The department is happy. If he didn’t end up escalating, I’m happy I did in fact get my unit, but I still feel guilty that I didn’t help him. If he did end up escalating because of not getting his water fast enough, I feel absolutely hideous.
==========
I quickly learned through fieldworks that I am not able to handle a job with productivity units. I would have been fired quickly. I get too stressed out about it. Too much worst case scenario thinking and too hard of a time saying no (or if I do say no, I obsess). I need to work on those issues, I do know that!
There are tons of very ethical therapists who work quite successfully in placements with productivity, obviously. I always wish I could be inside their heads to see what it would feel like to not go into worst case scenarios or always feeling bad about sometimes having to say no. Like in the situation above. I obviously went into worst case scenarios.
Luckily the American Occupational Therapy Association (AOTA) has been addressing the issues of productivity and ethics in our field – helping ensure that productivity standards are realistic and don’t lead to increased likelihood of ethical dilemmas, for example.
My occupational therapy capstone project is complete!
I wrote mine on “Increasing Awareness and Acceptance of Children with Disabilities Using Picture Books.” My Capstone Paper
I write about the importance of awareness and acceptance of children with disabilities, and how children’s picture books can serve as a form of disability awareness, which can promote acceptance, and therefore social inclusion…which ultimately leads to increased participation in occupation, which is the whole point of occupational therapy.
In addition, I talk about how OTs should consider incorporating picture books into their practice, and also how OTs should consider writing their own children’s books! It furthers the Centennial Vision, is a form of occupational justice, utilizes our unique talents, is in alignment with the Framework-III, and also has bonuses, on the business side of things. So far only four OTs that I know of have written five children’s book that have OT in them or even disabilities at all. Karen Jacobs, famous OT of the world, has written two of them. I want to be in the top ten. 🙂 Of course books about children with disabilities exist, but not enough of them, especially high quality ones.
Business wise, selling high-quality children’s books that exist already is a way to make a few extra dollars. And selling, giving away, or recommending them, especially if they are your own books, can be a value-added service, promoting satisfaction and loyalty. They are great for marketing. And if you write your own, especially if done as an e-book, you can make some money…well assuming it’s successful. Although to warn you, children’s books are hard to write well, and illustrations are quite costly.
To learn more about the process, read my capstone manuscript…the process etc is near the end, you can find via Table of Contents.
Use the Contact Me button on my website or email me…my name karendobyns, on gmail.com, if you want to say anything, because I just switched servers and the spam is out of control. I have over 2,000 comments and I won’t see yours…I have to get it fixed. Ugh.
Anyway….I got an A on my capstone YAY and after the presentation I give in 45 minutes through GoToMeeting (I think that’s the name), I am done with all but a single reflective post worth 1 point. 🙂 Post-professional clinical doctorate of occupational therapy (OTD), here I come!
Cadillac OT versus Reality OT
A wonderful occupational therapist/educator wrote the following forum post on our OTD forum (we are getting our post-professional clinical doctorates in OT). I asked her permission to post it because it resonated. What we learn in OT school and what we discover in the real world are two different things – but we have to remember in the real world that what we learned in OT school is still a valid and burning flame within us we must nurture and allow to grow.
“I remember something that one of my professors once said: “What you get in OT school is the ‘Cadillac version of OT.” I didn’t really understand it at the time, but the idea has stuck with me and I have certainly seen it in my own career. A lot of what we learned in school is how it should be, but not necessarily how it is currently. But we needed to learn it that way if there is any hope of changing things going forward. Each of us are then charged with holding on to pieces of the “Cadillac version” that fit within our practice, working to change things in practice to fit more of that in, and adapting to what we cannot change.
I try to make my teaching fit that approach. We emphasize occupation-based practice a lot in our curriculum, and we do teach preventative care and wellness, which aren’t necessarily reimbursed or even being practiced where our students complete their fieldwork. But some of our students have been able to fit these things into the otherwise very limited medical model at their sites, and others have the desire to find practice settings in the future that will allow them to use these skills.” – J.D.
Impress your Occupational Therapy Professors…
I’m writing an article for AOTA’s OT Student Pulse on the “Top Ten Ways to Impress Your Occupational Therapy Professors,” loosely based on this post that I wrote eight! years ago. I asked my OT Facebook friends, especially the OT instructors, to contribute their own thoughts. Since I can’t incorporate them all into the upcoming article, I added them here.
“…My first focus with students, and any novice or expert occupational therapist is not the knowledge, as though that is important, I have always said that one of the most important things in occupational therapy is the ability to develop rapport with the client (client in the broad sense- patient; family; system, etc.)…. as this is imperative for any other part of the occupational therapy process to work. – K.H.
“…Having had numerous relatives and me do OT and PT, .I’d like to say That K.H.’s post is dead on and should be (as Ford used to say) Job Number One for all therapists.” – J.S., Client/Caregiver
“I have students ask me all the time—“how can I be successful on fieldwork as an OT?”. I pause and say… I can teach you balance scales, manual muscle testing, G codes, vision testing, what glioblastomas are, how to identify cognitive issues vs psych issues, how to transfer people safely and how to document… What I can’t teach you is how to care, how to really see your patients, how to value each person and what they can teach you, or that you can learn from EVERY interaction ( good or bad). I cannot teach you to show up on time or early, tuck in your shirt, wear a clean shirt, brush your teeth, and to show up prepared to do your very best each day. You have to want this, you have to want this because there are people who cannot do for themselves and who need a voice. Caring— I cannot teach you to care….. if you care— there is no limit to the goodness one can do!” – S.S.
“Be one of the first to ask a question that shows you’ve done the required reading (reference the page #) and that you truly would appreciate more information. (It helps to clarify your level of understanding for the professor and probably helps at least two other students who are more hesitant to attempt this risky behavior.) Bonus points if you ask a question based on an AJOT article related to that or previous day’s assigned reading.” – L.F.
“…Always assume that your educators have the best intentions in the decisions they make” – and that these decisions are made to help shape you (and your peers) to become occupation-centred, flexible, reflexive, adaptable occupational therapists, who will be our future colleagues… and the future leaders of our profession! Whether you believe this to be true or not – coming from this standpoint when you open a discussion, ask a question or even query a grade means that you come from a position of respect and it will most likely then be responded to with respect.” – A.H.
“Demonstrate that you have an open mind and are willing to see things from different perspectives.
Get involved in your online community of practice …and not just for putting your assignments questions online and expecting someone to give you the answer. Hint. There isn’t usually one answer , it’s about showing you’ve thought about it, read around and made a clinically reasoned decision.
When reflecting. Be honest, and please reflect with purpose, to learn something.” – K.S.
“This was a good set of “ways to impress.” As I move into only my 6th year of teaching OTA students, I think it is important for students to learn to be persuasive — build a rational and compelling case for course of action when advocating for themselves or others. I prefer students to be slightly skeptical about the information that they are learning yet are polite about questioning the status quo of any particular system. I hope to encourage the creation of solutions, not only the identification of problems….”- B.C.